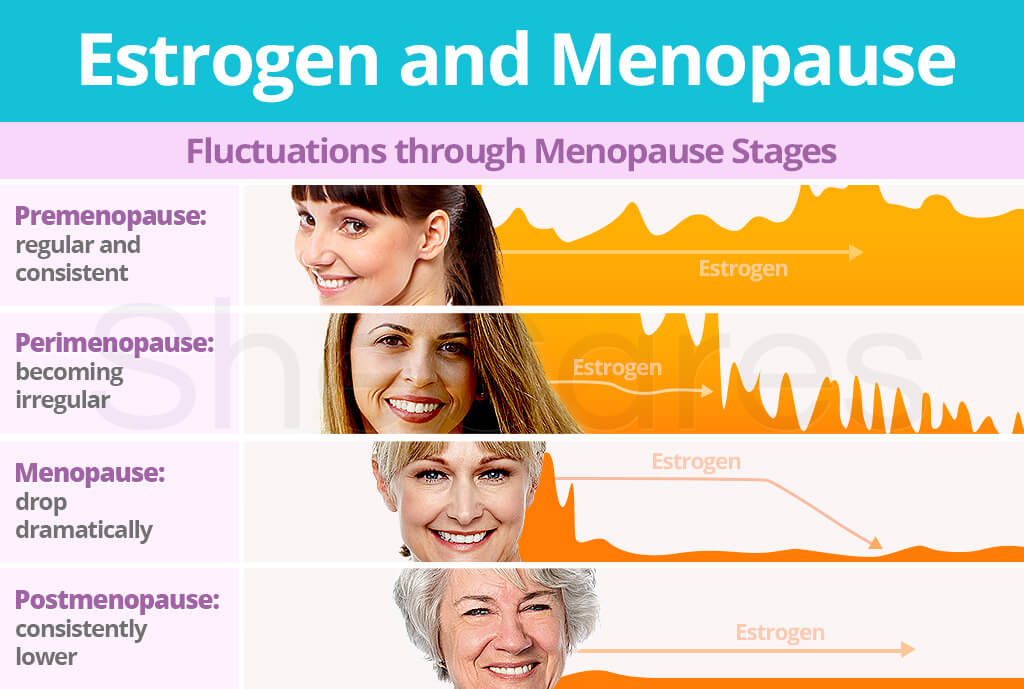
PREMENOPAUSE
PERIMENOPAUSE
POSTMENOPAUSE
It is important to pay attention to lifestyle changes and medical measures to maintain good health and quality of life.
The hormonal changes that occur during menopause, especially the drop in estrogen levels, have a significant impact on cardiovascular health. Estrogens are important in maintaining blood vessel elasticity, cholesterol balance, and protection against atherosclerosis, a condition characterized by thickening and clogging of the arteries. Decreased estrogen production during menopause leads to changes in the cardiovascular system and an increased risk of disease.
Estrogens stimulate the production of nitric oxide (NO) in the vascular endothelium, helping the blood vessels to relax and dilate, thereby reducing blood pressure and improving blood flow. As estrogen levels decrease, NO production decreases, which can lead to vasoconstriction and increased blood pressure.
In addition, estrogens regulate the lipid profile in the blood by increasing the level of high-density lipoprotein (HDL) or "good" cholesterol and decreasing the level of low-density lipoprotein (LDL) or "bad" cholesterol. As estrogen levels decrease, HDL decreases and LDL increases, increasing the risk of atherosclerosis. Atherosclerosis can lead to coronary heart disease, stroke, and peripheral artery disease.
During menopause, the decrease in estrogen also promotes inflammatory processes that contribute to the development of atherosclerosis. Inflammatory mediators such as C-reactive protein (CRB) are often elevated in the blood of postmenopausal women, which is associated with an increased risk of cardiovascular disease. Inflammation promotes the formation and instability of atherosclerotic plaques, which can lead to acute coronary events such as myocardial infarction.
Also, the lack of estrogen affects the structure and function of blood vessels. Estrogens stimulate the synthesis of elastin and collagen, proteins that support the structure and elasticity of blood vessel walls. Their deficiency can lead to stiffening of blood vessels and reduced elasticity, contributing to hypertension and increased workload of the heart.
For these reasons, the risk of cardiovascular diseases in women increases significantly during menopause. This highlights the importance of early prevention and proper health care during menopause, including regular medical examinations, healthy lifestyle, dietary control and, if necessary, medical treatment. Hormone replacement therapy may be considered in some cases to reduce menopausal symptoms and the risk of cardiovascular disease, but its use must be carefully evaluated for potential side effects and risks.
Arteriosclerosis, also known as atherosclerosis, is a process in which the walls of the arteries thicken and harden due to the buildup of fat, cholesterol, and other substances, forming plaques. This process begins when the inner layer of blood vessels (endothelium) is damaged by various factors, such as high blood pressure, smoking, high cholesterol, diabetes.
Fats, especially low-density lipoproteins (LDL), begin to accumulate at the site of damage, which are absorbed into the artery walls.
Over time, these fats oxidize and trigger an inflammatory response. Immune cells such as macrophages migrate to the site of damage to remove the oxidized fat. However, when fat accumulates, macrophages can overcrowd and turn into what are known as foam cells, which cause further inflammation and plaque formation. The plaques become thicker and harder as connective tissue and calcium grow into them. This causes the arteries to narrow and lose their elasticity.
This causes the arteries to narrow and lose their elasticity. When arteries become narrowed, blood flow to organs and tissues is reduced, causing a variety of health problems. First:
Atherosclerosis can also affect the peripheral arteries, causing peripheral artery disease (PAD):
In addition to physical consequences, atherosclerosis is associated with increased activation of inflammatory and immunological responses in the body, which can worsen overall health. This is especially true for those with other chronic diseases, such as diabetes or chronic kidney failure, as these conditions are often associated with the progression of atherosclerosis.
To reduce the risk of blood vessel blockage, it is important to follow a healthy lifestyle:
Medical care, including medications to control cholesterol and blood pressure, can also help slow the progression of atherosclerosis and reduce the risk of cardiovascular disease.

# menopauzė # aterosklerozė