WHAT IS DIABETIC NEUROPATHY?
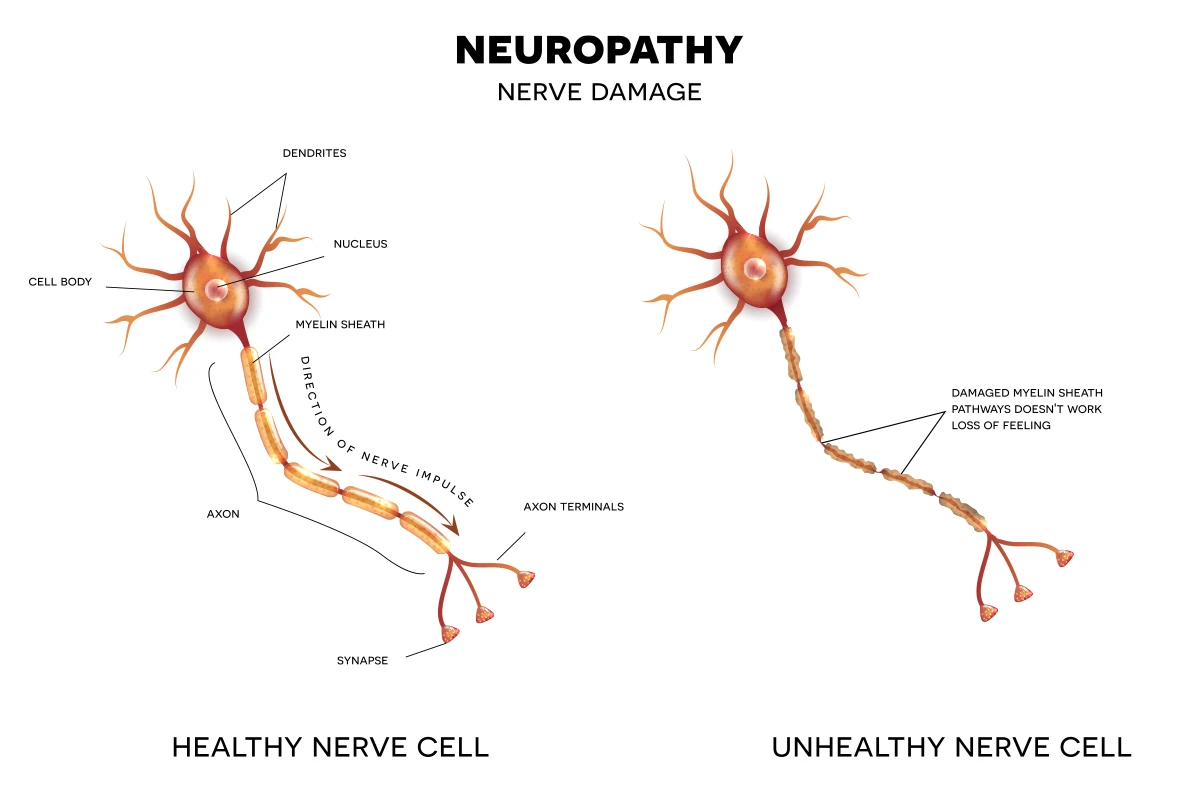
Diabetic neuropathy is a condition in which prolonged elevated blood glucose levels damage nerve fibers. Glucose essentially “poisons” nerve cells - it disrupts energy metabolism, accumulates in nerve tissues, causes oxidative stress, triggers inflammatory processes, and damages tiny blood vessels (microangiopathy) that supply the nerves. Over time, these processes lead to the degeneration of nerve fibers, impairing the transmission of signals between the brain and the limbs.
There are several types of neuropathy:
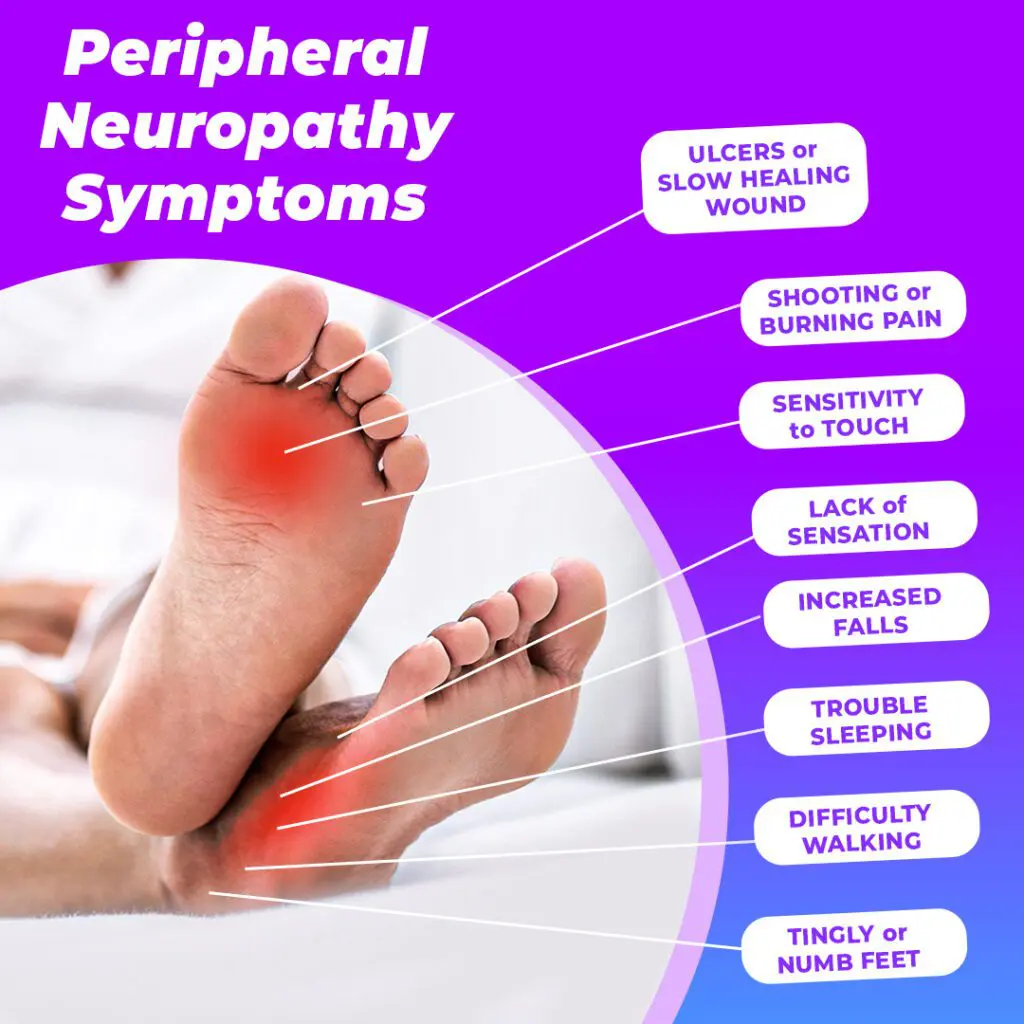
The feet are among the first and most frequently affected areas, as the long nerves that reach the feet are particularly sensitive to fluctuations in blood sugar levels.
Numbness in the feet is often perceived as a "minor issue" because it doesn’t cause active pain. However, pain is the body’s natural defense mechanism - a signal that tissues are injured. When this warning signal is lost, a person may unknowingly injure themselves and remain unaware of it for a long time. One of the most common situations is when a patient cuts, burns, or rubs their foot raw, but because they don’t feel pain, they continue walking on it. The wound becomes infected, an ulcer forms, and if circulation is also impaired (a common coexisting complication), the healing process slows down significantly, allowing bacteria to spread deeper - into tendons, bones, or joints.
In clinical settings, patients often first arrive with already purulent ulcers or gangrenous tissue damage, even though they report no pain at all. Loss of sensation also contributes to abnormal gait, balance disturbances, and a higher risk of falls - especially in older adults. So, this seemingly “harmless” symptom conceals much more serious dangers, which is why it must be actively monitored and managed.
The diagnosis of neuropathy involves both clinical evaluation and specific diagnostic tests. A diabetologist or neurologist will first ask the patient about symptoms such as numbness, burning sensations, “pins and needles,” loss of sensitivity to heat or pain, or difficulty maintaining balance. Then, objective sensory assessments are performed:
In certain cases, especially when symptoms are severe or progressing rapidly, additional electromyographic tests (EMG, NCV) are recommended to objectively measure nerve conduction.
Annual screening for signs of neuropathy is essential, even if no symptoms are present. Early detection allows timely intervention.
Although nerve damage is usually irreversible, its progression can be slowed or halted, and pain and discomfort can be significantly reduced. Effective neuropathy management consists of several key components:
Blood glucose control – the most important measure
Chronic high blood glucose levels (hyperglycemia) are the primary cause of nerve cell damage. Research shows that strict glycemic control can reduce the risk of new nerve injuries by up to 60–70%. This involves:
Daily foot care
Because patients may not feel injuries, feet must be inspected daily without exception. This includes:
Physical activity
Active movement improves microcirculation, helping small blood vessels deliver more oxygen and nutrients to nerve tissues. Recommended activities include:
Medications to relieve symptoms
For burning pain or “pins and needles” sensations, the following may be prescribed:
Other approaches
Some patients experience symptom relief with additional support measures:
# neuropatija # diabetas