Why does a spinal hernia occur?
When the hernia presses on nearby nerves, it can cause pain, numbness, or weakness. The pain can spread to the arms or legs, depending on the location of the hernia in the spine. For example, a hernia located in the neck area often causes pain and numbness in the hands, while in the lumbar area – in the legs.
Diagnosis includes a physical examination and imaging diagnostic methods, such as magnetic resonance imaging (MRI) or computed tomography (CT), which help determine the location and size of the hernia. Treatment can be conservative, including pain management with non-steroidal anti-inflammatory drugs (NSAIDs), physiotherapy, or, in more severe cases, surgical intervention.
It is important to mention that the onset and symptoms of a spinal hernia can vary greatly among individuals, and in some cases, a spinal hernia can be asymptomatic and detected during examinations for other reasons. Prevention of spinal hernia includes a healthy lifestyle, regular exercise, proper posture, and weight control.
What stages does a spinal hernia have?
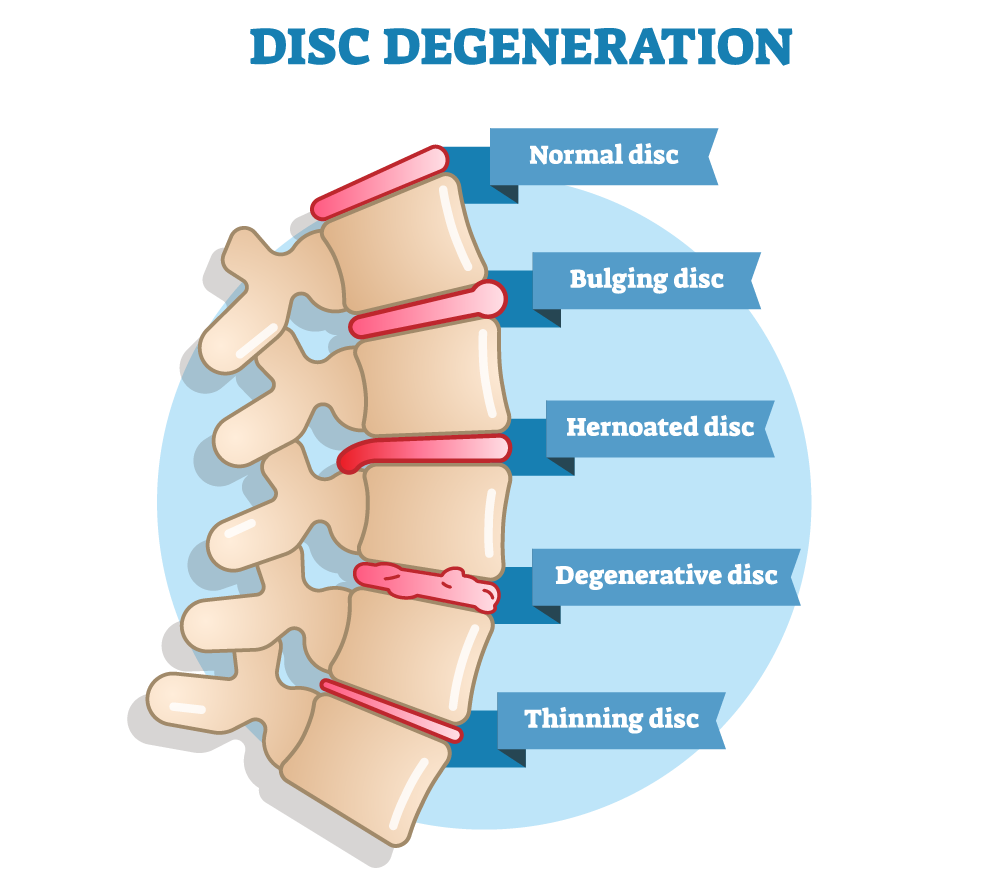
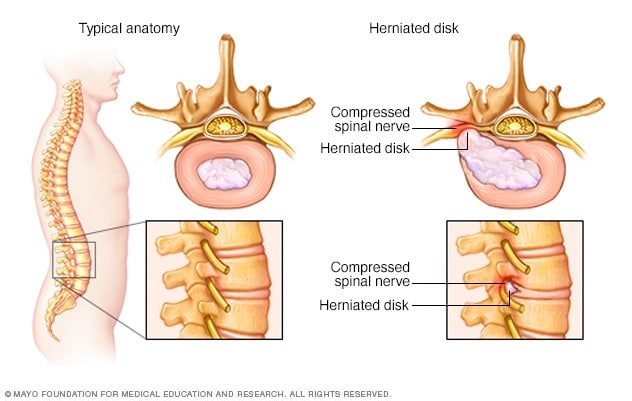
Spinal hernias, or intervertebral disc hernias, are a condition in which a part of the spinal disc protrudes or bulges, potentially causing nerve compression and pain. This condition can progress through several different stages:
- Disc desiccation: This is the initial stage, where the spinal disc begins to undergo degenerative changes. The disc becomes less flexible due to the loss of fluid, and its inner nucleus part begins to experience pressure. At this stage, patients may feel minimal discomfort or have no symptoms.
- Protrusion: At this stage, the disc begins to bulge, but its annulus (the hard outer part) has not yet ruptured. Protrusion causes increased pressure on surrounding tissues and can activate nearby nerves. Patients may experience pain, numbness, or weakness, depending on the location of the hernia in the spine.
- Herniation: This is the stage when the disc protrudes so that its soft nucleus part ruptures through the fibers of the annulus. This can cause more intense pain, especially if the spinal hernia presses on nearby nerves. Hernias can occur in any part of the spine, but most commonly occur in the lumbar region.
- Sequestration: The most advanced stage of herniation, where the disc material separates from the main disc and can move within the spinal canal. This condition can cause severe pain and even neurological disorders, such as leg weakness or urinary and fecal incontinence if the spinal hernia presses on the main nerves.
In each stage, treatment methods can vary, starting from conservative methods, such as non-steroidal anti-inflammatory drugs, physiotherapy, and exercise, to more innovative procedures, such as epidural steroid injections or surgical removal of the hernia. It is important to diagnose and treat a spinal hernia early to avoid long-term health problems.
Why does a spinal hernia occur?
A spinal hernia occurs when the soft inner part of a spinal disc, known as the nucleus, breaks through the disc's hard outer layer, known as the annulus. This is a complex condition that arises due to a combination of various factors.
Degenerative processes
One of the main factors in the development of spinal hernia is the natural aging process. As they age, the intervertebral discs, which act as shock absorbers between the vertebrae, can lose moisture and elasticity. This reduces their resilience and flexibility, making them more susceptible to damage.
Physical stress and trauma
Intense physical activity, improper lifting, sudden movements, or trauma can increase pressure on intervertebral discs. These activities can cause disc ruptures or annular protrusion, especially if the discs are already weakened due to degenerative changes.
Genetic predisposition
Research shows that genetics may play a significant role in the development process of a spinal hernia. Some people may have a genetic predisposition to weaker discs or a greater susceptibility to disc degeneration.
Weight and lifestyle
Overweight or obesity can increase pressure on the spine and discs, especially in the lumbar region. A sedentary lifestyle and weak back and abdominal muscles can also contribute to increased spinal load and the risk of developing a hernia.
Smoking
Smoking is associated with increased disc degeneration. Nicotine can disrupt blood supply to the discs, reducing their ability to regenerate and maintain adequate moisture levels.
Non-ergonomic posture
Prolonged poor posture, especially when sitting at a work desk or using a computer, can cause back muscle strain and increase pressure on intervertebral discs. This can cause or exacerbate disc degeneration and the risk of developing a spinal hernia.
The development of a spinal hernia is a gradual process, and not everyone experiencing degenerative disc changes will develop a hernia. However, understanding the risk factors and managing them can help reduce the risk of developing a spinal hernia.
Symptoms
Symptoms can vary depending on the location of the hernia in the spine and its size, as well as which nerves are affected.
The most common symptom is pain, the nature and intensity of which can vary greatly. The pain can be localized directly at the site of the hernia, for example, in the back or neck, and can spread to other parts of the body, depending on the nerve that is compressed. For instance, a lumbar hernia can cause pain that spreads into the leg (sciatica).
When the hernia affects the nerves, there can be sensations of numbness, tingling, or weakness in the corresponding body parts. For example, if the hernia is in the lumbar area and affects the outer leg nerve, numbness or weakness can occur in one or both legs.
Pain and discomfort can limit movement, especially in the mornings or after prolonged sitting. Certain postures or movements can exacerbate the pain.
In more severe cases where the hernia strongly affects the nerves, functional disorders can occur, such as urinary incontinence or difficulty controlling bowel movements. These are rare but serious symptoms that require urgent medical attention.
Prolonged nerve compression can cause muscle atrophy or weakness.
Some patients notice that their symptoms fluctuate – there may be better periods when symptoms are less felt, and worse periods when pain and other symptoms are more intense.
Symptoms of a spinal hernia can be similar to those of other back health problems, so it is important to consult a healthcare professional for accurate diagnosis and appropriate treatment. Early treatment can help prevent the worsening of symptoms and help maintain a quality lifestyle.
How is a spinal hernia treated?
Treatment of a spinal hernia is a complex process, focused on reducing pain, decreasing nerve compression, and improving overall spinal function. Treatment strategies depend on the size and type of the hernia, the symptoms it causes, and the overall health condition of the patient. Treatment usually begins with conservative methods, and surgical intervention is considered only when other methods are ineffective.
Conservative treatment
- Medication: Nonsteroidal anti-inflammatory drugs (NSAIDs) may be prescribed to reduce pain and inflammation. Sometimes, muscle relaxants or stronger pain relievers may be recommended for severe pain.
- Physiotherapy: A physiotherapist can prescribe special exercise programs to strengthen the back and abdominal muscles, improve flexibility, and reduce pain. Various physiotherapeutic procedures, such as ultrasound, electrotherapy, or heat and cold therapy, are also used.
- Exercise and kinesitherapy: Regular exercise, especially exercises aimed at stabilizing the spine and strengthening the muscles, can help reduce symptoms and prevent the recurrence of the condition.
- Chiropractic and manual therapy: Some patients may benefit from chiropractic or manual therapy procedures to improve spinal movement and reduce pain.
- Epidural steroid injections: Injections made directly into the spinal epidural space can help reduce inflammation and pain.
Surgical treatment
- Microdiscectomy: This is the most commonly performed surgery for treating spinal hernias. During the procedure, the surgeon removes the hernia, thus reducing pressure on the nerves.
- Laminectomy: A procedure in which a part of the vertebral bone is removed to increase the space in the nerve canal and reduce nerve compression.
- Fusion: Spinal fusion surgery is performed to join two or more vertebrae together, stabilizing the spine.
Lifestyle correction
- Weight control: Weight reduction can reduce pressure on the spine and alleviate symptoms.
- Ergonomics and posture correction: Proper posture and an ergonomic workspace can help reduce spinal load and pain.
- Nutrition and hydration: A balanced diet and adequate water intake can help maintain a healthy spine condition.
It is important to note that treatment should be individualized, considering the specific needs and health condition of the patient. Additionally, it is important to consult with healthcare professionals to create the most appropriate treatment plan. Treatment of a spinal hernia requires patient engagement and commitment to a long-term health care plan.
What sports can be practiced with a spinal hernia?
Engaging in sports with a spinal hernia requires caution and proper preparation. Appropriate physical activity can help strengthen back muscles, improve flexibility, and overall health, but it is important to avoid sports that can increase pressure on the spine or cause sudden, unwanted movements. Here are some types of sports that are often recommended for people with a spinal hernia:
- Hiking or brisk walking: Gentle, yet consistent movement, such as hiking or brisk walking, is an excellent choice. It helps strengthen the cardiovascular system without overloading the spine.
- Swimming and water aerobics: Swimming is one of the best options, as water reduces the effect of gravity and allows movement without significant pressure on the spine. Water aerobics can also be beneficial, as water provides additional resistance and helps strengthen muscles.
- Cycling: Cycling, especially on specially adapted stationary bikes, can be a safe choice. It is important to choose the right bike position to avoid additional pressure on the back.
- Yoga and pilates: These exercises help strengthen the abdominal and back muscles, improve flexibility, and assist in controlling breathing. It is important to choose gentle yoga or Pilates exercises and avoid positions that can increase spinal load.
- Back strengthening exercises: Specially designed exercises to strengthen the back muscles can be very effective. These exercises should be performed cautiously and preferably under the supervision of a specialist, such as a physiotherapist.
- Tai Chi or other slow martial arts: Tai Chi or similar slow martial arts can help improve body balance, coordination, and muscle strength, as well as reduce stress.

It is important to emphasize that any engagement in sports should be started after consultation with a healthcare professional, such as a doctor or physiotherapist. They can help determine the most appropriate level of physical activity and provide recommendations, considering the individual's health condition, the specifics of the spinal hernia, and overall physical condition. Additionally, it is important to pay attention to body signals and immediately stop the activity if any pain or discomfort arises.
Information sources:
- Mayo Clinic
- WebMD
- Healthline
- National Institutes of Health (NIH)
- The American Academy of Orthopaedic Surgeons (AAOS)
# stuburo išvarža